Cautionary and Advisory Labels (CALs)
Cautionary and Advisory Labels (CALs) are small yellow stickers that pharmacists add to your medicine. They provide critical safety messages to help you take your medicine correctly and minimise side effects or interactions. These labels are specific to your medicine. Don’t ignore them!
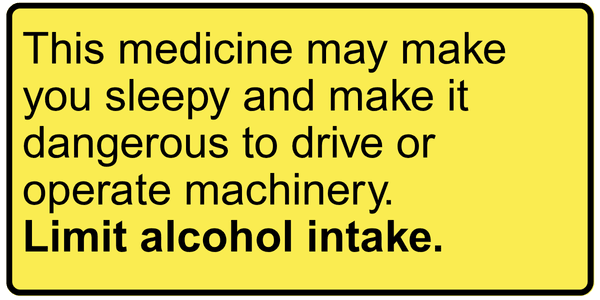
This medicine may make you sleepy and make it dangerous to drive or operate machinery. Limit alcohol intake.
This is used on medicines that can cause drowsiness and affect your coordination and reaction time. It doesn’t mean you must avoid driving or using machinery altogether; the warning is there to remind you that this medicine can affect your ability to undertake tasks safely. Alcohol can worsen these side effects. Taking multiple medicines with this label, and/or those with a warning about alcohol, can further increase the risk of drowsiness, poor coordination, and slower reactions.
Why does this label matter?
These effects can increase the risk of accidents and injury, not just for the person taking the medicine, but for those around them. If patients or their whānau are unaware of these effects, they may put themselves or others at risk of harm.
What can you do?
Use extra caution if you’re taking other sedating medications, recreational drugs, or have just changed the dose of your medicine.
If possible, take your first new or changed dose when you don’t need to drive or operate machinery so you can see how it affects you.
Let your friends or whānau know you’re taking a medicine with these effects so they can keep an eye out to make sure you are safe.
Discuss any concerns with your pharmacist.
Visit the NZTA website for more information. https://nzta.govt.nz/safety/driving-safely/medication/#:~:text=The%20consequences%20of%20taking%20medication,injure%20yourself%20or%20other%20people.
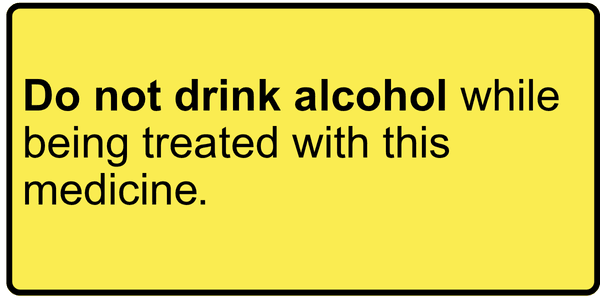
Do not drink alcohol while being treated with this medicine.
This is used on all medicines where alcohol should be avoided. Alcohol can increase drowsiness, alter the breakdown of the medicine, or the medicine can change the breakdown of alcohol, causing significant adverse effects.
Why does this label matter?
The effects of mixing alcohol and medicines are hazardous and even life-threatening. Alcohol and drugs can affect people in different ways; as little as one standard drink can increase sedation and impact coordination.
What can you do?
Avoid drinking alcohol while taking this medicine and for a few days afterwards.
Use extra caution if you have just changed the dose of your medicine.
Discuss any concerns with your pharmacist.
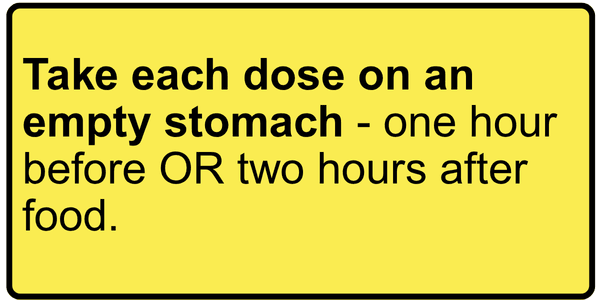
Take each dose on an empty stomach - one hour before OR two hours after food.
This is used on medicines that don’t work well if taken close to mealtimes. When you're hungry and before you eat, your body releases acid into the stomach. Stomach acid breaks down some medicines, so they won’t work.
On the other hand, there are medicines that are irritating to the stomach or are more effective when taken with food. When this is the case, your label will include this instruction.
Why does this label matter?
Following this label helps ensure your medicine works properly and gives you the best possible results. Here is an example of how to take your medicine around mealtimes.
What can you do?
Set reminders on your phone to remember to take your medicine or take it with you if you need to take it during the day.
Discuss any concerns with your pharmacist; we can help you plan a schedule to minimise disruption and get the best benefit from your medicine.
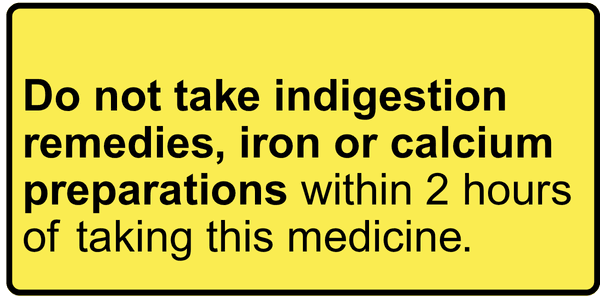
Do not take indigestion remedies, iron or calcium preparations within 2 hours of taking this medicine.
This is used on medicines that may not work if taken too close to products containing iron or calcium, such as antacids, iron supplements, or calcium supplements. This includes products such as Gaviscon, Mylanta, Quick-Eze, and Acidex, as well as some vitamins and supplements, and even calcium-rich foods in some instances (milk, cheese, yoghurt). This warning does not apply to these medicines: omeprazole, pantoprazole, or famotidine.
Why does this label matter?
When taken at the same time as the medicine, these substances bind to the medicine, preventing it from being absorbed into the body and reducing its effectiveness.
What can you do?
Wait at least 2 hours before or after taking your medicine before taking these other products.
Consult your pharmacist, as we can provide advice on reflux and indigestion.
Discuss any concerns with your pharmacist.
Avoid certain foods and alcoholic drinks.
This is used on specific medicines that interact with certain foods and drinks. This is a rare warning, typically used for monoamine oxidase inhibitors (MAOIs) medicines such as tranylcypromine (Parnate). If you are taking one of these medicines, talk to your pharmacist about how to stay safe while taking your medicine.
https://www.mayoclinic.org/diseases-conditions/depression/expert-answers/maois/faq-20058035

KEEP IN FRIDGE - DO NOT FREEZE.
This is used on medicines that need to be stored in the fridge between 2°C and 8°C to stay effective. These medicines may be damaged if they become too warm or freeze.
Why does this label matter?
Medicines are made with ingredients that can break down or change if they’re stored at the wrong temperature. This can cause:
The medicine to lose strength or change in its texture or appearance, so it may not work correctly.
Safety issues such as from the contamination of bacteria.
What can you do?
Store your medicine in the centre of the fridge, away from the door, freezer, or back wall. This keeps the temperature more stable.
Don’t use medicines that have been frozen or appear different from their usual appearance. Check if the packaging feels frozen, solid or if the medicine has changed in appearance.
Discuss any concerns with your pharmacist. They can help you determine if the medicine is still safe to use or if it needs to be replaced.
Do not use after .../.../…
This label means your medicine has a specific expiry date after it has been opened or made up in the pharmacy. Always check this date and stop using the medicine after that point, even if there’s some left.
Why does this label matter?
Some medicines lose their effectiveness once opened or mixed. Over time, they can:
Lose strength, making them less effective.
Break down into new compounds, which might be harmful.
Become contaminated, especially liquids like eye drops
- Eye drops are at higher risk because each use exposes them to air and bacteria. Over time, preservatives break down, and bacteria can grow inside the bottle.
What should you do?
Don’t use a medicine past the date on the sticker or bottle.
Don’t keep opened eye drops or liquid medicines for future use.
Check the label or ask your pharmacist if you’re unsure how long your medicine lasts after opening.
Return all expired or unused medicines to the pharmacy for safe disposal.
Discuss any concerns with your pharmacist.
Protect yourself from too much natural or artificial sunlight while being treated with this medicine.
Some medicines can cause severe light sensitivity reactions when people are exposed to sunlight. This is not sunburn, but it can present in many ways and severities. Some reactions occur straight away after sun exposure (phototoxic reactions), and some develop up to two days later (photoallergic reactions). These reactions can occur from new medicines and medicines that you have had before.
These rashes can vary in appearance and severity, but they may resemble severe eczema and can cause intense burning, itching, blistering, and crusting. Reactions typically occur when there is direct exposure to light (on the arms, face, and neck). Depending on the severity of the response, this rash can spread to other parts of the body.

Why does this label matter?
It is impossible to predict an individual’s response to a light-sensitive medicine or how common a reaction will be, a warning label is included for medications that have been shown to cause these reactions.
What can you do?
Remember SLIP, SLOP, SLAP, and WRAP?
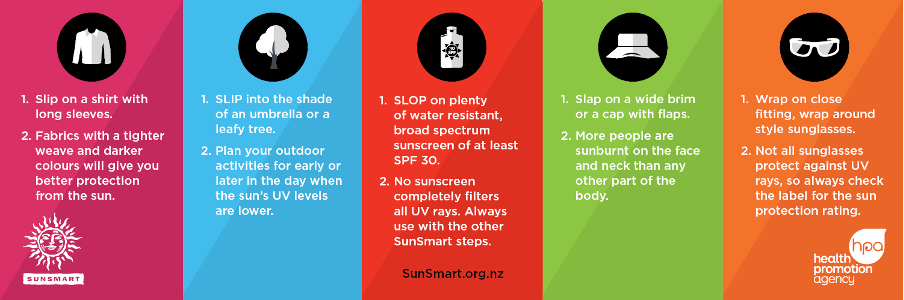
This is the best way to protect yourself and decrease the likelihood of getting a reaction from the sun or artificial light.
Avoid artificial lights such as sunbeds, and be careful when getting your nails done at the salon with UV light lamps.
Be careful even on cloudy days and in the winter. Any exposure to sunlight or light can trigger a reaction.
Discuss any concerns with your pharmacist.
Do not stop taking this medicine without consulting your doctor.
This is used on medicines where it is essential not to stop taking them suddenly, even if you feel better or think you no longer need them. Suddenly stopping some medicines can be dangerous.
Why does this label matter?
Your body adapts to certain medicines and stopping them suddenly can cause rebound effects or withdrawal symptoms. This is especially important for:
- Antidepressants or anxiety medicines
- Heart or blood pressure medicines
- Corticosteroids (like prednisone)
- Epilepsy medicines
What can you do?
Always consult your doctor before stopping any medication with this warning.
Don’t stop taking your medicine completely, even if you’ve missed a dose.
Discuss any concerns with your pharmacist.
Take each dose with a large glass of water.
This is used on medicines that, if stuck in your throat or oesophagus (food pipe), can cause pain and damage.
Why does this label matter?
While all tablets and capsules should be taken with water while sitting or standing upright, this label is used when there is an added risk of damage to your throat or oesophagus (food pipe) if they don’t go down properly.
What can you do?
Take all medicines with a full glass of water (about 200–250 mL) to help them reach your stomach safely.
Sit or stand upright while taking your medicine, and ideally, remain in this position for 30 minutes afterwards.
If any medicines get stuck in your food pipe, then try to eat soft foods such as breads or bananas to try and help push it down.
Discuss any concerns with your pharmacist.
Seek urgent medical attention if you experience coughing up blood, dark or coffee-ground–coloured stools or any unusual bleeding or signs of irritation in the throat or stomach.
Grapefruit or grapefruit juice may interact with this medicine. Discuss with your pharmacist.
This is used on medicines where grapefruit (and its juice) can affect how the medicine works. Grapefruit blocks enzymes in your gut and liver, which break down many medications. Blocking this effect can cause your medicine to accumulate in your body, resulting in unpredictable or unwanted side effects.
Why does this label matter?
Even small amounts of grapefruit juice (200 mL) can cause problems, and the effects can last for over 24 hours. The severity of the interaction can vary from person to person and is dependent on many factors. Because these effects are variable and unpredictable, it’s safest to avoid grapefruit juice entirely if your medicine carries this warning.
What can you do?
Avoid grapefruit and grapefruit juice by being aware of what is in what you're consuming.
The other fruit that can cause this effect are pomelos and Seville oranges, commonly found in some marmalades.
Choose safe alternatives such as navel oranges and mandarins.
Discuss any concerns with your pharmacist.